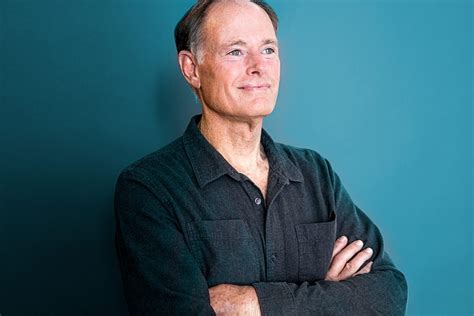
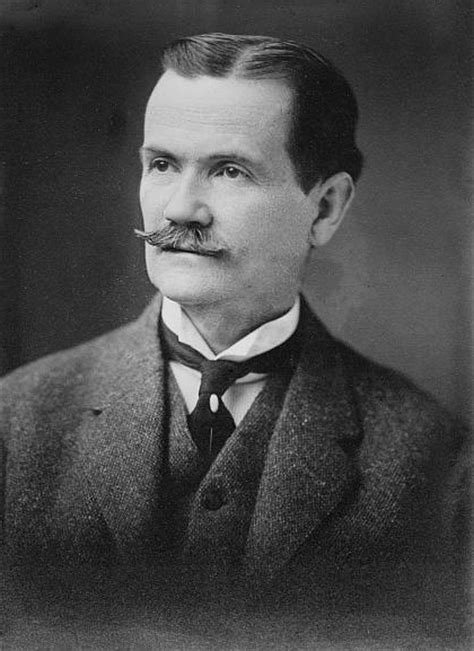
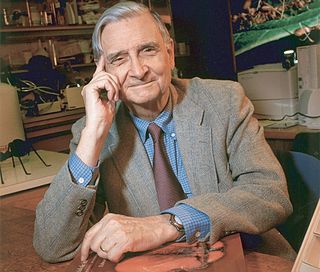
A Quote by David Perlmutter
As a practicing neurologist, I can tell you first hand that working with Parkinson's patients offers clinical challenges. But from an emotional perspective, this disease can border on overwhelming.
Related Quotes
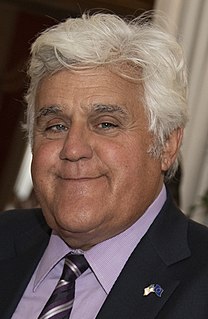
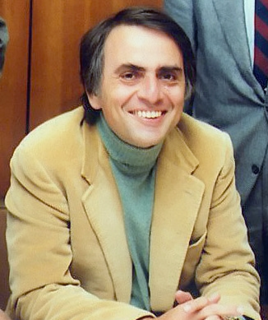
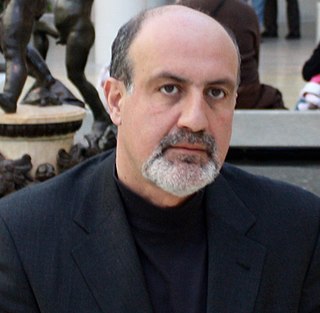
It seems The Journal of Neurology reports that the longer you smoke, the less likely you are to develop Parkinson's disease. So what are they telling us? Follow me guys. Remember, a couple of months ago, doctors said drinking a glass of alcohol every day was good for your heart. Smoking prevents Parkinson's disease. Marijuana is good for glaucoma. Sex is good for your prostate. You know, screw health care. Let's party!
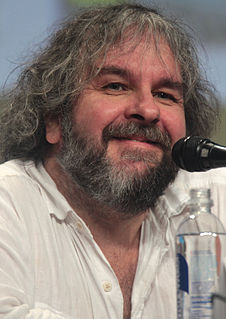
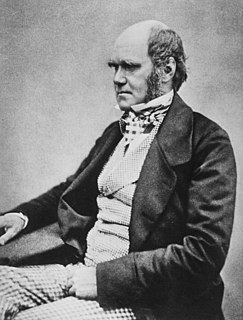
The rhythm of music is very, very important for people with Parkinson's. But it's also very important with other sorts of patients, such as patients with Tourette's syndrome. Music helps them bring their impulses and tics under control. There is even a whole percussion orchestra made up exclusively of Tourette's patients.