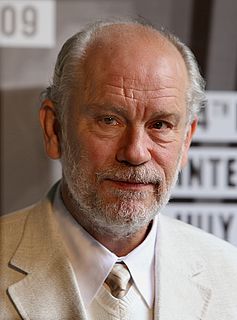
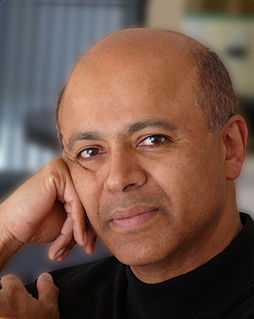
A Quote by John Malkovich
I'm not a psychiatrist. I'm not treating patients.
Quote Topics
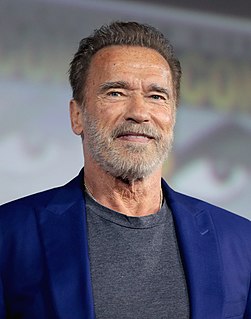
Related Quotes
Treating only terminal cancer patients, the Rand (anti-cancer) vaccine produced objective improvement in 35% of 600 patients while another 30% demonstrated subjective improvement. FDA stopped the vaccine's use in a federal court hearing where neither the cancer patients nor their doctors were allowed to testify.
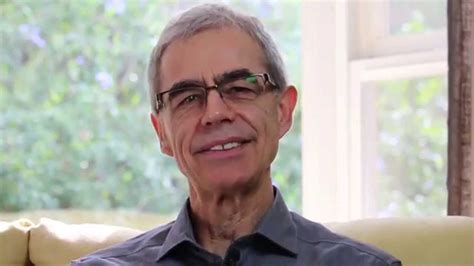
The need of an insecure psychiatrist to draw security from a virtuous adjustment to the conventionalities of his time and from a quest for approval from "the good and the great" may turn out to be another agent interfering with his ability to listen in a therapeutically valid fashion. This type of dependence gives rise to the danger that the psychiatrist may consider the changeable man-made standards of the society in which he lives to be eternal values to which he and his patients must conform.
There are a very small number of doctors in France that use essential oils and herbs as well as conventional drugs in their treatments and sometimes they will use essential oils intensively, usually because they are treating people with cancer or chronic infections that patients have had for years, and ingested essential oils are a really a great choice for treating chronic infections if you're a doctor.
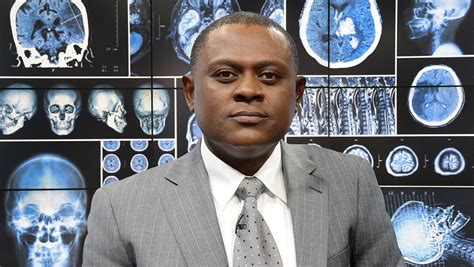
I am a spiritual person. I'm a Catholic. I treat my patients, the dead patients, as live patients. I believe there is life after death. And I talk to my patients. I talk to them, not loudly but quietly in my heart when I look at them. Before I do an autopsy, I must have a visual contact with the face.