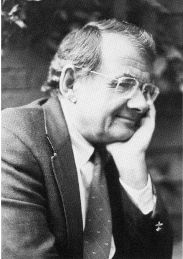
A Quote by Robert Fischell
It takes an average of three hours after the first symptoms of a heart attack are recognized by the patient, before that patient arrives at an emergency room. Symptoms are often denied by the patient - particularly us men, because we are very brave.
Related Quotes
What do we know about autism in 2013? Autism symptoms generally emerge before age three and usually much earlier, often as language delays or lack of social engagement. Recent research suggests that autism can be detected during the first year of life, even before classic symptoms emerge. Indeed, the symptoms may be a late stage of autism.
A patient doesn't select his physical ailments. They happen to him. You could just as well ask when you are eaten by a crocodile, 'How did you select that crocodile?'. Nonsense. He has selected you. The patient doesn't even select the symptoms unconsciously. That is an extraordinary exaggeration of the subject to say he was choosing such things. They get him.
Imagine someone who has had a heart attack on the street, and they are picked up by an ambulance with 5G connectivity, hi-definition scanners, and cameras... You start taking a scan in the ambulance so all of that data is transferred to the surgery before the patient arrives, and a diagnosis is already underway.