A Quote by Tommy Tuberville
PBMs claim they help patients by negotiating lower prices from drug manufacturers. But the fact is PBMs rarely, if ever, pass those savings on to patients.
Quote Topics
Related Quotes
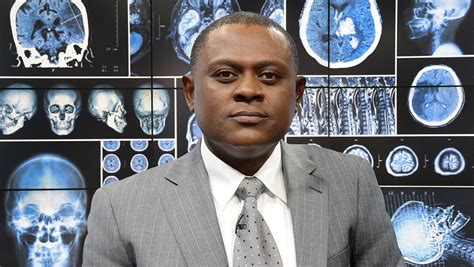
I am a spiritual person. I'm a Catholic. I treat my patients, the dead patients, as live patients. I believe there is life after death. And I talk to my patients. I talk to them, not loudly but quietly in my heart when I look at them. Before I do an autopsy, I must have a visual contact with the face.
Pretty much everybody knows there are not enough organs for all of those patients who need to get transplants, and what happens is, is that organs are actually directed in liver transplantation to those patients who are the sickest. So the patients who have the greatest chance of dying in the next three months or so are the ones who get the priority for the liver transplant.
When the FDA forces an old drug off the market, patients have very little say in the matter. Patients have even less of a say when the FDA chooses not to approve a new drug. Instead, we are supposed to rely on the FDA's judgment and be grateful. But can the FDA really make a choice that is appropriate for everyone? Of course not.
The survival rate of Dr Burton's patients approximately doubled the maximum survival rate of conventionally treated patients. Had these findings pertained to a chemotherapy drug instead of IAT, massive amounts of funding would have been allocated to investigate the drug. Once again, the politics of cancer barred a potentially valuable treatment from reaching the public.